Diagnosis & Management of MSMDS
DIAGNOSIS & MANAGEMENT
FOR MULTISYSTEMIC SMOOTH MUSCLE DYSFUNCTION SYNDROME
Potential Health Problems and Monitoring Recommendations*:
Neurological
10,11
- Changes in the brain vasculature are progressive and often lead to white matter injury, Transient Ischemic Attacks (TIAs), strokes, and seizures. Although the brain large vessel changes are frequently compared to Moyamoya Disease, there are distinct differences in those affected by MSMDS. Distinctive angiographic differences include dilation of proximal internal carotid arteries, an abnormally straight course of intracranial arteries, and absence of typical moyamoya collateral vessels. Injury to the brain from white matter disease or strokes can lead to developmental delays, seizures, excess fatigue, partial paralyzation associated with stroke, learning difficulties, hearing and language difficulties. In addition, individuals should be aware of the
early warning signs of stroke.

Figure 9. Neurological changes should be monitored throughout the lifetimes of those affected with MSMDS
Monitoring Recommendations Include:
- Neurological evaluation every 6-12 months performed at a Stroke Center when possible.
- Imaging of the brain and head/neck (preferably MRI) should be performed according to neurologist recommendation during neurological assessment at time of diagnosis and every 1-2 years depending on the type of symptoms. Computed Tomography (CT) Scans should be avoided if there are no current signs or symptoms of acute stroke.
- Transcranial doppler (TCDs) assessments every year to monitor progression of cerebral arterial narrowing.
- Avoid anesthesia or sedation when possible for imaging studies. Sedation can lead to lower blood flow to the brain and strokes due to lack of autoregulation.
- Neurocognitive assessments by pediatrician or neurologist should be performed every 12 months during childhood and adolescence.
- Formal neuropsychological evaluation should occur if either of the following are noted:
- Developmental delays or learning difficulties.
- MRI shows white matter injury or strokes
- Hearing evaluation should be performed at diagnosis and annually following diagnosis.
- Contact should be established with Vascular Neurosurgeon with expertise in MoyaMoya Disease or ACTA2.R179H.
- Hematological evaluation should be performed to assess risk of treatable clotting and bleeding that may prevent stroke.
- Rehabilitation specialists should be contacted if motor or sensory challenges are present.
- Electroencephalogram (EEG) should be performed if there are concerns of seizures.
- Catheter angiogram should be reserved for when MRA shows critical narrowing of the vessels and there have been signs/symptoms of stroke or TIA.
Possible Treatments (if needed):
- Consultation with stroke neurologist and cardiologist should occur prior to beginning new medications.
- Acetylsalicylic acid (ASA) 81mg (or 3-5mg/kg in children) daily if narrowing of the intracranial vessels is seen in the MRA and there is no bleeding.
- Good hydration is essential, especially when active and in hot environments.
- Seizure medications may be necessary if recurrent seizures are present.
- Medications may be necessary to treat low blood pressure if symptomatic.
- Revascularization surgery may be necessary to decrease the risk of stroke. This procedure carries a high risk of complication in MSMDS individuals. If considered necessary, consult cerebrovascular surgeon with experience in MoyaMoya disease.
Cardiovascular 11,12: The primary complications in the cardiovascular system include aortic widening and dissection, high heart rate, aneurysms in vasculature throughout the body, blood clots, and low blood pressure due to inability of veins and arteries to regulate blood pressure. Monitoring recommendations for those affected suggest that each person should:
- Be evaluated by their Cardiologist every 6-12 months.
- Have transthoracic echocardiograms every 6-12 months to monitor blood flow and aortic changes.
- Have imaging of the chest, abdomen, and pelvic vessels performed at the time of diagnosis and every 12 months starting at 10 years old (unless recommended more frequently by their doctor).
- In addition, individuals should be aware of the signs and symptoms of blood clots throughout the body which include swelling, pain, red or blue skin coloring, and/or heat and tenderness to the touch.
Possible Treatments (if needed):
- AT1 Angiotensin II receptor antagonist such as Losartan (as blood pressure allows).
- Vasopressors as required to maintain normal blood pressure levels.
- Replacement of ascending aorta or aortic grafting.
- Blood thinners if active clotting occurs in narrowed vessels. Consultation with neurologist is recommended if use of blood thinners is considered.
Pulmonary
11:
Complications in the pulmonary system include pulmonary hypertension, emphysema, chronic lung disease, asthma, and collapsed lung (pneumothorax). Those affected should undergo pulmonological assessment as needed and especially in the presence of infection. Although rare, some affected require additional breathing support which is exacerbated with illness. Individuals should be aware of the signs and symptoms of pulmonary hypertensive crisis. Caution should be taken to avoid unnecessary exposure to respiratory viruses. If severe respiratory distress occurs and critical care is needed, it is recommended that the intensivist and pulmonologist communicate with stroke neurologist to minimize risk of strokes during sedation needed during this crisis. Avoid high airway pressures when possible given under-septation of the lungs and risk for pneumothorax.
Gastrointestinal
11,13:
Complications in the GI systems include slow gastric emptying, gut malrotation, esophageal reflux, chronic constipation, and gallbladder distress. Some may require gastrointestinal tubes for proper nutrition and some are unable to eat orally due to esophageal reflux. Antacid medications may be indicated. Those with severe esophageal reflux are at increased risk of aspiration pneumonia. Due to gut and stomach malrotation, individuals with MSMDS should know the signs and symptoms associated with bowel obstruction to include abdominal pain, constipation, diarrhea, abdominal distention, and/or vomiting. Individuals should undergo gastrointestinal assessment at the time of diagnosis and as needed. Growth and nutritional assessment should be evaluated every 12 months during childhood and adolescence. A high fiber diet and good hydration can decrease constipation and improve gut motility.
Urological/Urogenital
11:
Complications in the urological system include hypotonic bladder, hydronephrosis, hydroureter, vesicoureteral reflux, recurrent urinary tract infections (UTIs), undescended testes, and hydrocele. Severity of kidney involvement depends largely on the ability of the bladder to remain empty to prevent fluid “back-up” into the kidneys (hydroureter and hydronephrosis). Some will need frequent catheterization to evacuate the bladder or a permanent bladder catheter. Those with more severe renal disease may require dialysis and/or transplantation. In addition, those affected may require a special diet to prevent excess strain on the kidneys. Bladder complications include inability to empty which leads to frequent infections which can become severe if left untreated. Lastly, undescended testes in males may lead to impaired fertility. Individuals affected by MSMDS should undergo urogenital assessment at the time of diagnosis and yearly thereafter, and should be aware of the signs and symptoms of UTI. Individuals diagnosed with subsequent Eagle Barrett Syndrome (commonly known as Prune Belly Syndrome) may incur additional urological, urogenital and gastrointestinal challenges.
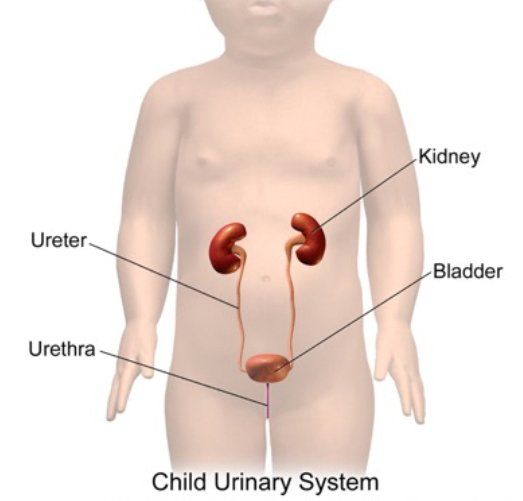
Figure 10. Child Urinary System Reflecting Path of Kidneys to Bladder
Ophthalmological - Complications involving the eyes include inability of the pupils to constrict, retinal vessel damage, and retinal detachment. Inability of the pupils to constrict prevents light blocking which may cause extreme light sensitivity. In addition, patients may have impaired ability to “accommodate” making focusing on objects at varying distances difficult. Progressive brain changes may also affect an individual’s level of eye function.
- Ophthalmological evaluation should be performed at diagnosis and annually after diagnosis.
- Use of sunglasses is recommended for UV protection and to improve quality of life.
- Optometrist evaluation recommended to assess need for corrective lenses to help with accomodation deficits.
- If a visual field deficit is suspected, consult with neurologist regarding possible brain injury.
*Not all patients experience the same presentation and challenges. Listed above are those that have been described to date for informational purposes only.
Prevention: Currently, there are no recommendations for prevention due to the genetic nature of the disorder, however awareness and proper clinical management may prevent or slow progression of the disease.
Screening and Diagnosis:
Three characteristics of MSMDS are common to all who are affected: Cardiac PDA, fixed and dilated pupils, and brain changes seen with imaging. If at least two of these signs are present, screening should occur. Those affected, however, will likely have other signs and symptoms in addition. DNA sequencing is required for exact diagnosing and to rule out other genetic mutations in the ACTA2 gene (see Table 1 for specific mutations). In addition, 17% of known MSMDS cases are affected subsequently by Eagle Barrett Syndrome (PRUNE BELLY SYNDROME) which requires additional intervention.

Familial Genetic Testing: With most genetic disorders, there is concern for possible concurrent diagnosis with other children in the family. In most cases of MSMDS, the disease occurs due to a genetic mutation that occurred spontaneously (de novo) during the development of the sperm or eggs and thus affects the baby, but is not present in any other cells of the parents (Figure 12, Left ). To date, one case of familial MSMDS has been discovered, where the faulty gene was passed from an undiagnosed parent to infant. Children who are affected will have a 50/50 chance of passing the disorder on to their own offspring (Figure 12, Right) Since this genetic mutation is spontaneous (de novo) most frequently, siblings of the child are not typically affected. However, there is still much to be discovered. Full genetic screening may be recommended for the entire family of those affected given the largely unknown nature of MSMDS and
ACTA2 Mutations.
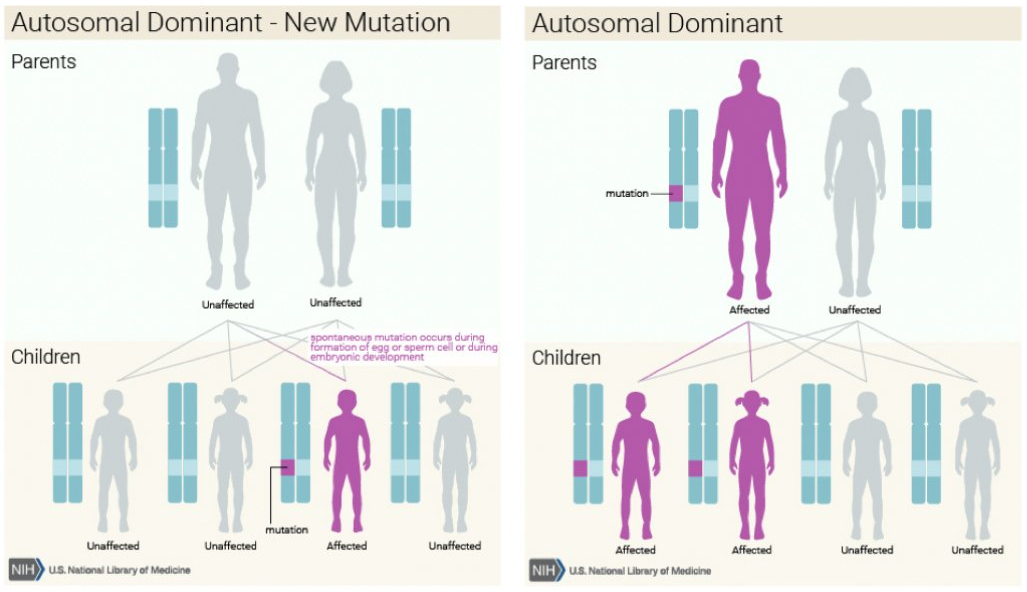
Figure 12. Familial Inheritance Pattern of Autosomal Dominant Genes
Collaboration:
A recently published GUIDE TO CLINICAL MANAGEMENT has provided physicians with some assistance in common findings, imaging recommendations, and potential treatment options. Due to the rarity of this disease, very few physicians have experience in management and treatment of MSMDS. It is imperative that all members of the child’s healthcare team are aware of current recommendations, and identify the importance of collaboration when it comes to clinical decision making.